Why vaccination strategy is not as simple as it seems
September 14, 2021
When vaccination just started getting underway in the U.S., many people were confused and angered at the fact that many localities were pursuing vaccination strategies that didn’t just boil down to vaccinating the most vulnerable. On the other hand, there was a significant movement to vaccinate front-line workers which often cited equity and racial justice as motivations. What didn’t seem to make the news as often is the mathematics that make this a reasonable alternative to consider.
The strategy of vaccinating those most likely to suffer adverse outcomes from COVID-19 is intuitive: we first protect those most in need of protecting. Of course, when we phrase it this way, we see a slight chink in the logical armor—while those with pre-existing conditions and the elderly are definitely more likely to suffer adverse outcomesNote that I am explicitly not limiting this to death. As noted previously, there are a host of other reasons to want to avoid getting COVID, these consequences are also dependent on their risk of being exposed to the virus.
Key concept: diseases spread along contact networks
Key to understanding why there might be considerations beyond the health status of each individual is the realization that we are all interconnected through a web of interpersonal interactions. In disease ecology, we call this a “contact network.” Directly communicated diseases such as COVID Most recent research suggests that spread through virus particles persisting on shared surfaces is rare for COVID, especially outside of hospital settings rely on the innate sociality of humans to spread from one host to another. What actually counts as a “contact” will depend on the properties of the pathogen in question: we all have heard the “at least 15 minutes of less than 6 feet proximity” rule-of-thumb for COVID, but for influenza, it might take more time or shorter distances, while the delta variant of COVID might be able to spread further or faster. Importantly, these are all based on probability distributions and unlucky individuals might get infected over much longer distances or just passing by an infectious individual. Similarly, someone not getting infected after spending a day with an asymptomatic carrier does not disprove the general trend.
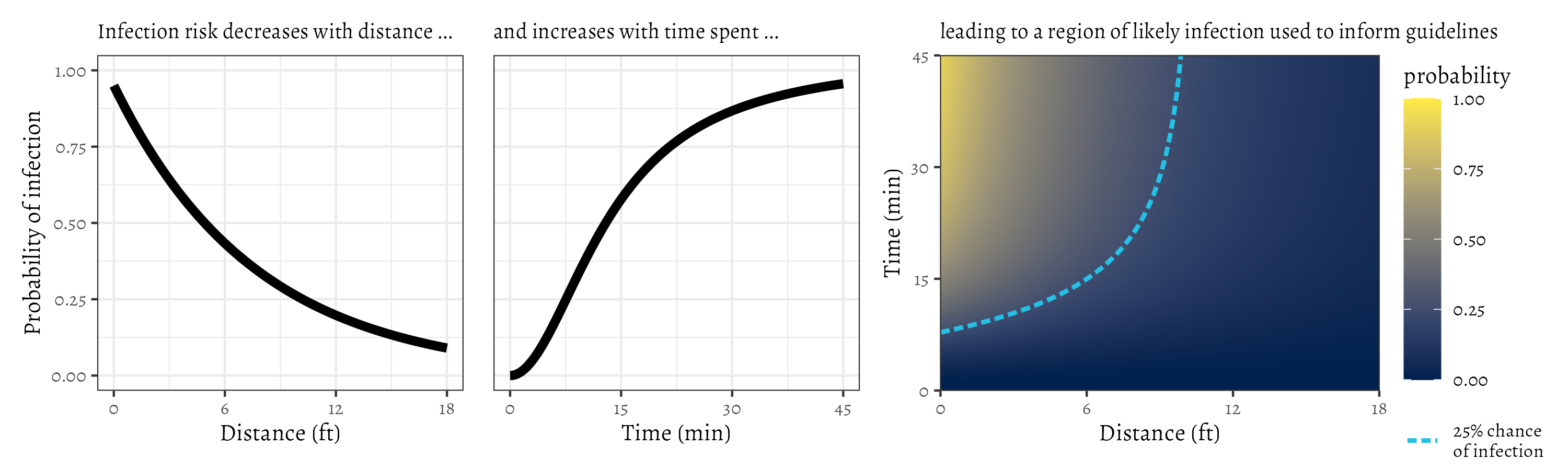
Here is a conceptual diagramThat is, figure not meant to represent actual data, but rather to help us think about a problem of what these guidelines are trying to capture:
Note that there is some probability of being infected in any given moment that depends on the distance you are from an infectious person. Similarly, the longer you are near that person, the more likely you are to get infected yourself. The guideline is a way of simplifying the message that, for example, you have a 1 in 4 chance of being infected by the time you have spent 15 minutes within 6 feet of an infectious person (the upper-left region of the heatmap inside the blue curve).
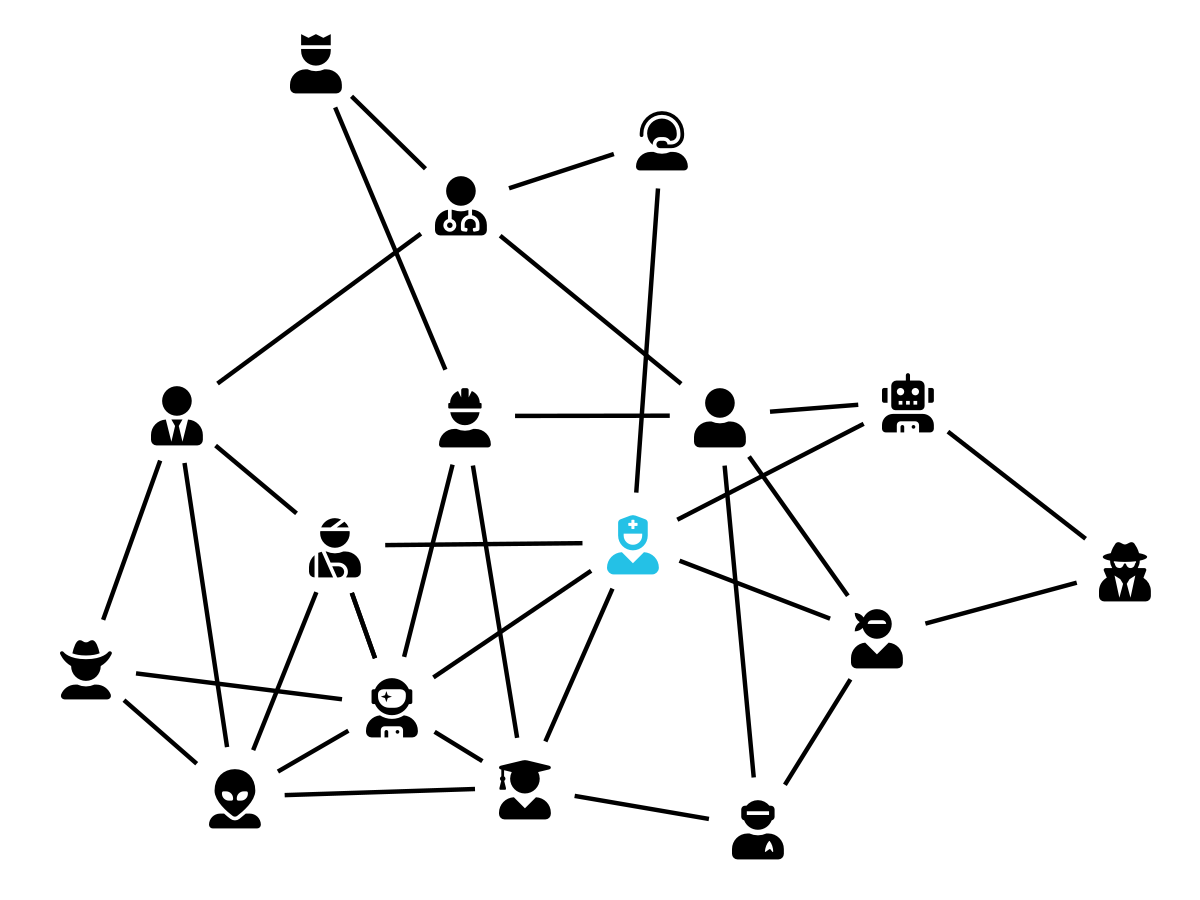
When we consider every interaction between every pair of individuals in a population (possibly even varying through time), we end up with data that can be visualized as a network, where the “nodes” are individuals, and the “links” are interactions that have the potential to spread disease. Because diseases spread along this network of interactions, we can begin to see how vaccinating certain individuals (such as the blue nurse at the center of our plotted network) can have a disproportionate impact on the spread of disease. This effect can be further amplified when a person’s job involves a risky behavior in addition to a large number of interpersonal interactions (consider, for example, dentists, whose work involves increase exposure to aerosolized particles and interacting with many people in close contact and for extended periods of time).
An alternative: vaccinating to reduce disease spread
So, how do we operationalize this network perspective? Put simply, a network view of vaccination suggests we should additionally consider both exposure risk (the risk of being infected) and spread risk (the risk of passing the pathogen along to others)For a fun, interactive exploration of this idea, check out this game. In it, you have a limited number of vaccines to distribute amongst a population to minimize the total epidemic size. It doesn’t consider differential vulnerability, but does a good job of demonstrating the importance of contact network structure on the spread of disease.
Thinking about differential risk of exposure and spread across the population is complicated because it depends on many interacting variables, such as the prevalence of disease within the population, the personal behavior of people when they are interacting with one another, and even environmental features such as airflow. The factor that we are focusing on here for the sake of vaccine distribution, is how each person fits within the wider social contact network: a person who largely stays home and minimizes their contact with others has a low risk of being infected and is unlikely to contribute to further disease spread even if they do happen to get sick; a waiter, delivery person, or teacher, on the other hand, has both a higher likelihood of being infected and of passing that infection along to others as a result of their position within the contact network. Thus, it might make sense to prioritize these “high risk” people for vaccination, reasoning that reduced disease spread might result in lower morbidity and mortality in the population as a whole.
But which is the better course?
Thus far, I’ve focused on explaining an alternative to the health-status approach to vaccination, using contact network structure as a conceptual framework, but, with the obvious caveat that this is not a dichotomous It is not a choice between two exclusive options (like True/False, Black/White, etc.); there are hybrids and alternatives not discussed here choice, how should we be administering vaccinations in response to COVID-19?
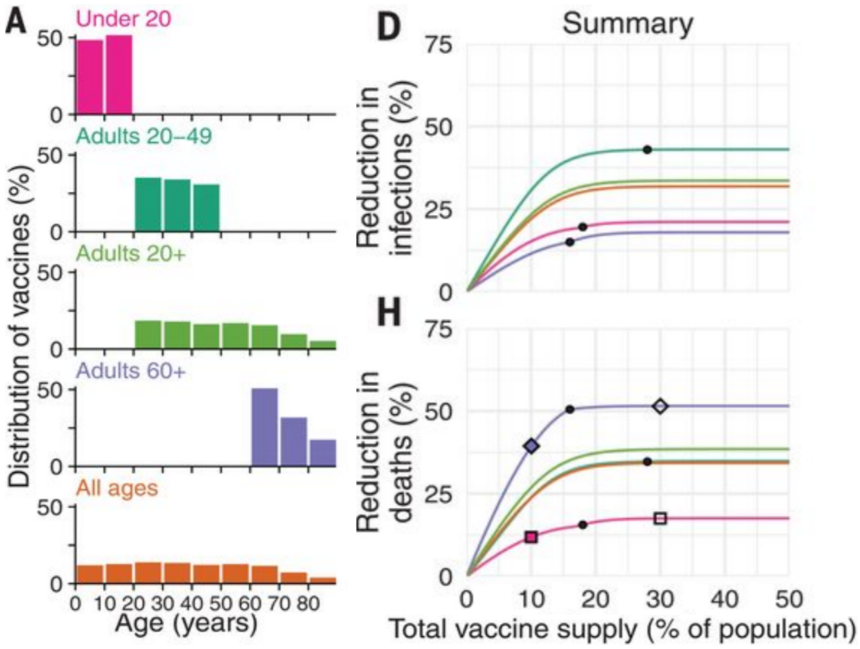
A recent studyBubar, et al. Science 2021 looking into this question for COVID-19 found that the approach of vaccinating the more vulnerable is better if your goal is to minimize deaths.
Some subset of readers are at this point exclaiming that “of course! this was obviously going to be the result,” and are probably wondering why they’ve wasted their time reading this whole post.THANK YOU!, by the way It is important to remember that this didn’t have to be the case. In fact, in the same study, they found that targeting younger people (who both make up a larger fraction of the population and are more likely to interact with others) had a greater effect on reducing the overall case-burden.
If we were considering another disease with a less dramatic connection between age and mortality rate, this reduction in overall case number might be enough to shift the mortality results to favor this approach as well. It is also worth mentioning that the study is only considering mortality directly caused by COVID-19, while there is ample evidence that overburdened health care systems have morbidity and mortality costs outside of this narrow definition: many people that need medical care cannot or do not get the care they need when hospitals are full of COVID patients, even if most of those patients will not die from the disease.
Figure modified from Figure 1 of Bubar, et al. 2021. Note that the largest reduction in deaths (highest curve in the bottom-right (H)) corresponds to preferentially vaccinating the elderly. The curves in the top-right (D) indicate reductions in total number of COVID-19 cases. For this outcome, vaccinating younger individuals (those 20-49 years old) has the largest effect.
So, at least in part, the answer to which policy is better depends on your priorities, as well as a proper quantification of the many externalities of increased daily new COVID case counts. Intuitions are not always correct, and we need to do the research to be confident in our choices, especially when there are lives on the line.